Medical professionals are urging the public to separate fact from widespread fiction regarding the human papillomavirus (HPV), a common infection that nearly everyone encounters. While often harmless, persistent infection with certain high-risk strains is a leading cause of cervical cancer, making understanding and routine screening critical.
Demystifying a Common Virus
HPV is a family of viruses that infect skin and mucosal tissues, with numerous subtypes identified by numbers, explains Adeola Olaitan, a consultant gynaecological oncologist at The Wellington Hospital, part of HCA Healthcare UK. The virus spreads through any genital skin-to-skin contact, meaning penetrative sex is not necessary for transmission; it can pass via vaginal, anal, or oral sex and shared sex toys.
Contrary to popular fear, most infections are transient and cause no symptoms or long-term harm. "In most cases, HPV is a transient, harmless condition, and most people clear it without even knowing that they had it," says Olaitan. The immune system typically eliminates the virus naturally within two years.
Olaitan highlights a significant misconception: the stigma linking HPV to promiscuity. "People think it has connotations of promiscuity, which it doesn't. You can have sex once and get HPV," she states, emphasising that the association with sexual activity should not lead to shame or unnecessary anxiety.
Understanding the Link to Cancer Risk
Of the over 200 known HPV strains, they are categorised as low-risk or high-risk. Only a small proportion are linked to cancer. According to Cancer Research UK, around 14 strains are considered high risk for cervical cancer, with two in particular posing the greatest threat.
HPV types 16 and 18 are responsible for approximately 70% of all cervical cancer cases. "HPV 16 and HPV 18 can infect the cervix, and if the infection persists then they can increase the risk of cervical cancer," Olaitan clarifies. The key risk factor is a persistent infection, not the initial exposure itself.
Since HPV usually presents no symptoms, individuals are unlikely to know they have it without screening. "The knowledge of whether you have HPV or not is only important because it marks people out as having a greater risk of having abnormal cells," Olaitan notes. If these cellular changes are left unchecked, they can develop into cancer over many years.
Prevention Through Screening and Vaccination
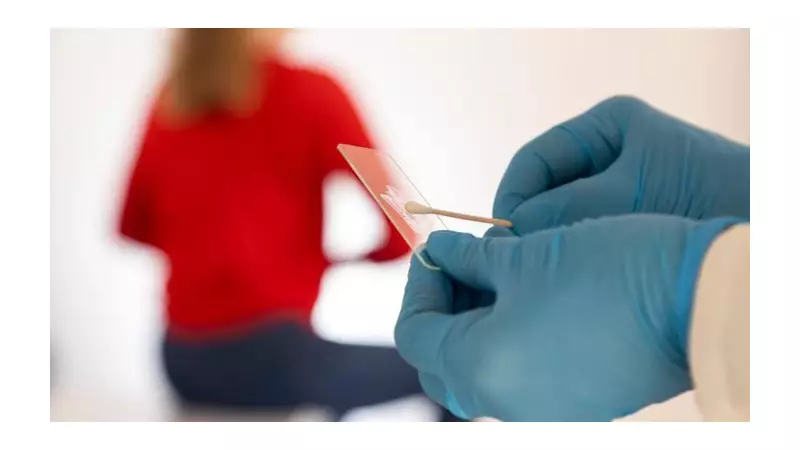
The NHS cervical screening programme is a frontline defence. It invites all individuals with a cervix aged 25 to 64 for a test every five years, checking cells for high-risk HPV strains.
Olaitan outlines the process: "If the initial screening finds high-risk HPV, a reflex cytology test would be conducted on the same sample. If abnormal cells are found you will be referred for a colposcopy to have a closer look at the cervix."
Vaccination offers powerful protection. The HPV vaccine is routinely offered to children aged 11 to 13 and is licensed for use up to age 45. "The HPV vaccine is very effective at protecting people against HPV," says Olaitan, though she adds that it is less effective the older you are, as it works best before exposure to the virus.
However, vaccination can still be beneficial even after exposure. "You can have it even if you've been exposed to HPV or you have a current HPV infection. It gives immunity that's stronger and longer lasting than natural immunity alone," she explains.
Being aware of potential symptoms is also crucial. Olaitan highlights the most common signs of cervical cancer: bleeding after sex, bleeding between periods, bleeding after menopause, or an offensive, persistent vaginal discharge. While these often indicate less serious conditions, they should always be checked by a doctor to exclude cancer.
The expert message is unequivocal: "Remember that cervical cancer is preventable, and people who go for regular screenings are unlikely to get cancer." Combining the knowledge that HPV is usually harmless with the proactive steps of attending screenings and considering vaccination forms a robust strategy for long-term health.