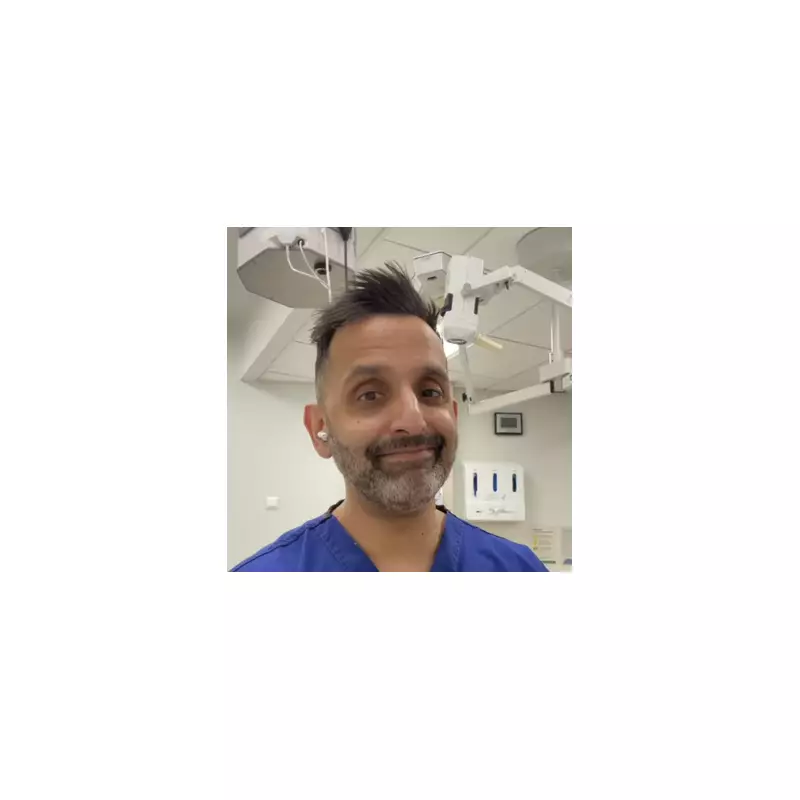
Television doctor Amir Khan has provided a detailed explanation for why numerous women frequently wake up experiencing stiffness and soreness in their joints, particularly as they approach midlife. The full-time GP and resident medical expert on ITV's Lorraine and Good Morning Britain has highlighted a specific condition often referred to as 'menopause shoulder,' linking it directly to hormonal changes during the perimenopause and menopause stages.
The Role of Estrogen in Joint Health
In a recent video shared on his Instagram platform, Dr Khan emphasised that many women are mistakenly told that joint pain in midlife is simply a natural part of ageing. He clarified that estrogen plays a crucial and multifaceted role in maintaining joint health, which is often overlooked in general discussions about menopause symptoms.
Estrogen is vital for several key functions within the musculoskeletal system:
- It helps maintain collagen levels, which provide tendons and ligaments with their essential strength and flexibility
- It contributes to proper joint lubrication, ensuring smooth movement
- It helps keep inflammation under control throughout the body's connective tissues
When estrogen levels begin to decline during the perimenopause transition, these protective mechanisms become compromised. Tissues gradually become stiffer and less elastic, while joints lose their smooth movement capabilities. This physiological change explains why many women report suddenly feeling older, stiffer, and more sore upon waking, despite having felt considerably more mobile just a few years earlier.
Understanding Menopause Shoulder
Dr Khan identified one of the most striking manifestations of this hormonal impact as what's commonly called menopause shoulder. Medically, this condition is typically diagnosed as frozen shoulder, also known by its clinical term adhesive capsulitis. The doctor noted that this painful condition is significantly more prevalent among women around the time of menopause compared to other demographic groups.
The symptoms can be particularly debilitating in daily life:
- Simple tasks like putting on a coat or fastening a bra become unexpectedly difficult
- Reaching upward into cupboards or shelves often causes significant discomfort
- Nighttime pain frequently intensifies, especially when lying on the affected side
What makes menopause shoulder particularly frustrating for sufferers is that it often appears to develop without any obvious injury or trauma. The condition typically progresses through three distinct phases: an initial painful phase, followed by a period of extreme stiffness, and finally a slow thawing phase that can extend over several months before full recovery.
Management and Treatment Approaches
Dr Khan offered practical advice for women experiencing these symptoms, stressing that appropriate management requires a nuanced approach. While movement remains important for joint health, he cautioned that it must be gentle and carefully guided. Forcing the shoulder or pushing through sharp pain typically exacerbates the problem rather than providing relief.
Effective treatment strategies often involve multiple approaches:
- Professional physiotherapy sessions with targeted exercises
- Appropriate pain relief medications when necessary
- Patience, as the condition often requires considerable time to resolve
- For some women, addressing menopause symptoms more broadly through hormone replacement therapy, where medically appropriate, can help alleviate overall joint symptoms
The doctor emphasised that frozen shoulder often requires specific management tailored to its unique progression, even when broader menopause treatment is being implemented.
A Crucial Message for Women
Dr Khan concluded with an important message for women experiencing new joint pain during perimenopause or menopause. He urged them not to automatically attribute such symptoms to normal wear and tear or assume they must simply endure the discomfort without seeking proper medical evaluation.
Recognising that hormonal changes can have powerful effects on joints and connective tissue represents the essential first step toward obtaining appropriate treatment. By understanding the connection between estrogen levels and musculoskeletal health, women can advocate more effectively for themselves within healthcare settings and explore treatment options that address the root hormonal causes alongside the physical symptoms.