The National Health Service in England is set to undergo its most significant reorganisation in over a decade, with approximately 18,000 staff roles facing elimination as part of sweeping government reforms.
Following tense negotiations between NHS England and the Treasury, a £1 billion deal has been secured that will allow the health service to overspend this year to cover redundancy payments, with the amount to be recovered through future savings.
Major structural changes ahead
The transformation will see NHS England, the body responsible for day-to-day health service operations, absorbed directly into the Department of Health and Social Care. Simultaneously, local Integrated Care Boards (ICBs), which coordinate regional healthcare planning, are expected to reduce their management staff by half.
Health Secretary Wes Streeting defended the controversial measures, stating that both patients and NHS workers have consistently complained about a system that has become "too layered" and "too bureaucratic."
"People want to see the front line prioritised, and that's exactly what we're doing," Streeting told BBC Breakfast. "We're finally on the road to recovery."
Financial implications and government assurances
Ministers project that the restructuring will ultimately save £1 billion annually by 2028 – funding they claim could support approximately 116,000 hip and knee operations each year.
The government emphasises that no additional money is being injected into the NHS beyond the previously agreed £29 billion annual real-terms increase scheduled for 2028-29. Instead, officials argue that streamlining the service through these redundancies will generate long-term financial benefits.
In a scheduled speech to NHS managers, Streeting is expected to reassure taxpayers that every penny saved will be redirected toward improving patient care.
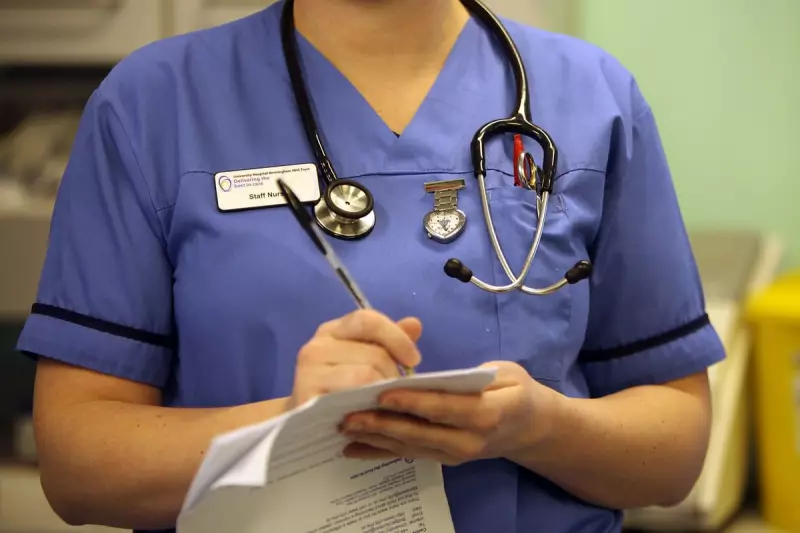
Concerns from healthcare professionals
Despite government assurances, healthcare unions and staff representatives have voiced significant concerns about the potential consequences of such extensive job losses.
Patricia Marquis of the Royal College of Nursing criticised the characterisation of affected staff as unnecessary administrators, stating: "Front-line services need more investment, but doing this off the backs of making thousands of experts redundant is a false economy."
Marquis emphasised that many of those facing redundancy are "experienced nurses and specialists who run vital programmes and connect the NHS with social care."
Daniel Elkeles, chief executive of NHS Providers, described the decision to proceed with redundancies as "pragmatic" but acknowledged the difficult position of staff who have demonstrated commitment to the health service only to face an uncertain future.
Health service insiders warn that the reorganisation is already causing disruption and distraction throughout the system at a time when the NHS continues to grapple with record waiting lists, workforce shortages, and rising patient demand.
The reforms reverse the 2012 establishment of NHS England under then Health Secretary Andrew Lansley, which was designed to provide the health service with independence from day-to-day political interference. Critics, including Lansley's successor Jeremy Hunt, had subsequently described the organisation as having become a "bureaucratic monster" that stifled innovation and local control.